Despite the enormous benefits of hepatitis B vaccination, it appears that this administration has its sights on changing the policy of administration at birth.
NY Times 9/16/25: C.D.C. Vaccine Advisers May Limit Hepatitis B Shots for Newborns
An excerpt:
Committee members, some of whom are vaccine skeptics, are likely to recommend restricting the use of the shots at birth or delaying them until later in childhood…
“Unless the mother is hepatitis-B-positive, an argument could be made to delay the vaccine for this infection,” Martin Kulldorff, the committee’s chair, said at its previous meeting in June.
Vaccine experts at the C.D.C., who normally would be deeply involved in preparing for this week’s meeting, have been sidelined and given no more information than the public about the meeting’s agenda or possible outcomes…
Before 1991, when newborns were not all vaccinated for hepatitis B, about 20,000 babies became infected each year. Routine immunization at birth cut the number of newborn infections … There are now fewer than 20 children per year who acquire the disease from their mothers.
Only about half of the cases before 1991 were a result of transmission from an infected mother. The other half “weren’t getting it from becoming sex workers, and they weren’t getting it from being intravenous drug users,” Dr. Paul Offit, director of the Vaccine Education Center at Children’s Hospital of Philadelphia, said…
From 2015 to 2017, about 21,000 infants were born to pregnant women with hepatitis B antibodies, but fewer than half were identified through prenatal screening, according to the C.D.C.
- Related news article: Jackie Fortier, NPR 9/16/25 Link to 3 minute report: RFK Jr.’s vaccine panel is expected to recommend delaying hepatitis B shot in kids “:”A vaccine advisory panel, recently reshaped by RFK Jr., is expected to vote on changing the age children should get their first hepatitis B vaccine — from right after birth to age 4”
- Jackie Fortier, NPR 9/16/25 Kennedy’s vaccine panel expected to recommend delaying hepatitis B shot in children Full length article
My take: If routine immunization at birth is stopped, there will be a lot more hepatitis B infections and subsequent complications. Some infections will be acquired at birth and some later due to missed opportunities to provide protection later on.
Related blog posts:
- Good News Story: The Remarkable Hepatitis B Vaccine Story
- Hepatitis B Vaccine Protects for Up to 30 Years
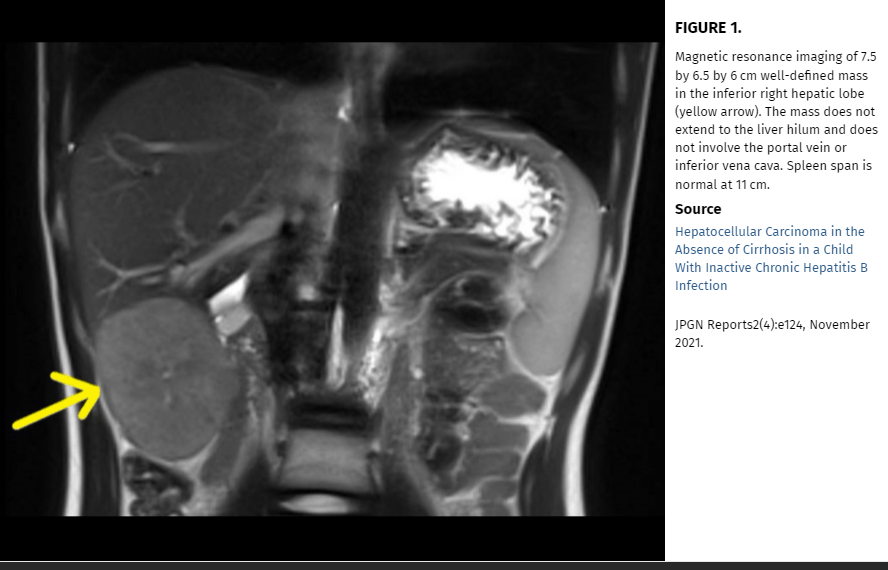
- Chronic Hepatitis B in North American Children …
- Antivirals Reduce Vertical Transmission of Hepatitis B …