In previous posts, this blog (see below) has examined the potential bias of studies reporting better outcomes in breastfed infants along with issues of maternal guilt. A recent commentary explores the issue of feeling guilty when breastfeeding does not go well.
AJ Kennedy. NEJM 2023; 388:1447-1449. Breast or Bottle — The Illusion of Choice
Some excerpts:
Only about 25% of women in the United States exclusively breast-feed for the recommended period.2 After my struggles, these statistics seem realistic to me, but before I went through it myself, I had no concept of how hard it could be…
Around the time my son turned 6 months old…my primary care doctor… gave me the courage to start taking medication and to stop breast-feeding that very week. Though the guilt about stopping has never fully gone away, the joy and happiness in my life quickly returned…
Even after I’ve told them that I might not choose to breast-feed this time around [with 2nd child], multiple doctors have “reminded” me that breast milk has been shown to carry Covid-19 antibodies — yet another reason to feel ashamed if I choose not to breast-feed…I am hopeful that this time around I can embrace formula feeding more quickly if that is the path that works best for me and my baby,…
I encourage the AAP and other national health organizations to consider how their statements on exclusive breast-feeding are perceived by the public. If 75% of us are not meeting this goal [6 months of exclusive breastfeeding], a more patient-centered approach and recommendation is needed.
My take: Breastfeeding does not work for everyone. Parents often feel guilty about perceived short-comings and we need to find a balance in encouraging breastfeeding but acknowledging that formula feeding is a good alternative.
Related blog posts:
- Feeling Guilty about Stopping Breastfeeding? Geoff Der, a statistician at the University of Glasgow who has worked with the same data in previous studies, said that the findings in the present study were robust and the authors’ method for eliminating selection bias was powerful…“In a society with a clean water supply and modern formulas,” he said, “a woman who isn’t able to breast-feed shouldn’t be feeling guilty, and the likelihood that there’s any harm to the baby is pretty slim.”
- Feeling Guilty about Stopping Breastfeeding? (Part 2)
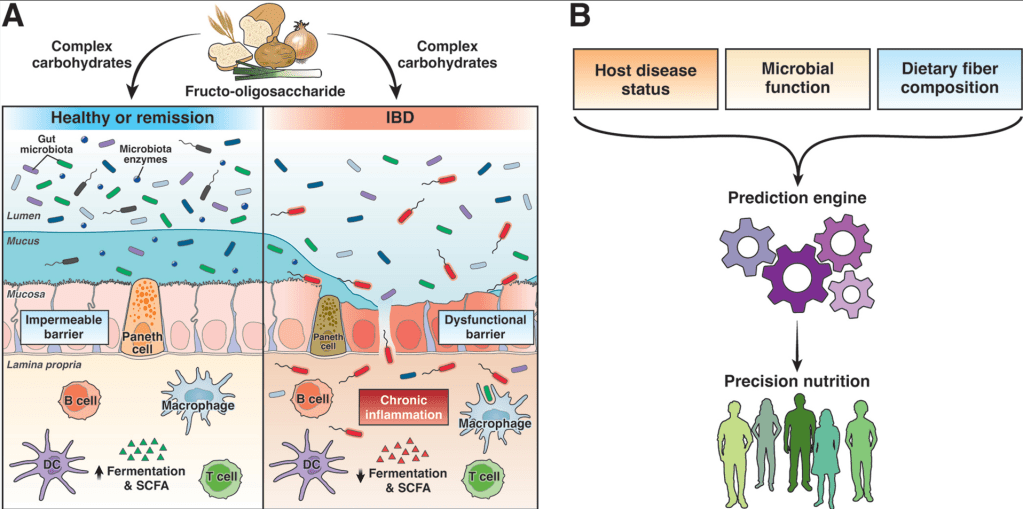
- Briefly Noted: Breastfeeding and Microbiome Diversity
- Breastfeeding and IQ -the Latest Data
- It’s Complicated: The Relationship Between Milk and Health
- Laying to Rest a Breast-Feeding Myth